Canavan disease is a relatively well characterized leukodystrophy, yet despite a basic understanding of the root cause of this fatal genetic disorder, the mechanisms whereby the genetic defect results in dysmyelination, brain vacuolation and neurodegeneration remain an area of intensive research. The genetic defect in CD results in a defective enzyme known as aspartoacylase or ASPA. ASPA has only one known function, to deacetylate the highly concentrated brain metabolite N-acetylaspartate (NAA). The primary reason for the lack of understanding of the mechanisms linking ASPA deficiency with dysmyelination and brain vacuolation lies in the lack of knowledge about the primary functions of NAA in the nervous system. NAA is synthesized in neurons, but ASPA is present mainly in oligodendrocytes, and it is known that NAA-derived acetate from neurons ends up in their ensheathing myelin. Therefore NAA appears to be a trophic molecule passed from neurons to oligodendrocytes where it is converted to acetyl coenzyme A (acetyl CoA).
Canavan Disease affects all populations, but the incidence in the Ashkenazi Jewish population is higher than most other populations, with 1 in 87 people of Ashkenazi decent being carriers of one of the more common gene mutations. The figures worldwide are unknown because many cases go undiagnosed. Genetic mutations that present with a milder form of Canavan disease have also been reported, and the carrier frequencies for these less severe mutations are also unknown. Canavan disease babies are normal at birth, but most show signs of developmental delay and muscle weakness within 3 to 6 months after birth. Muscle weakness becomes more pronounced as the infants develop, and normal feeding becomes difficult, and then impossible. Vision and hearing are severely affected, and eventually children develop seizures. Most children die before adolescence, but some with milder forms survive into their 20s and beyond. Current treatments are symptomatic only, including the use of feeding tubes and anti-epileptic agents.
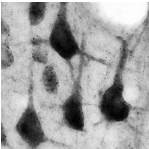
There are currently two contrasting hypotheses on the pathogenic mechanisms of CD. One hypothesis posits that the accumulation of excess NAA in the brain impairs osmotic regulation in neurons, or results in excitotoxicity. In contrast, we have hypothesized that NAA-derived acetate is a significant source of acetyl CoA (NAA being synthesized in neurons and transferred to oligodendrocytes) which in turn is used in the synthesis of fatty acids and for use in protein acetylation reactions such as histone acetylation. Under this hypothesis, a lack of ASPA activity in the brain causes defective oligodendrocyte maturation and myelin synthesis during the period of developmental myelination, leading to spongiform degeneration of brain in CD patients.